Introduction:
Philadelphia (Ph)-like B-cell acute lymphoblastic leukemia (ALL) is a high-risk subgroup of B- cell ALL with distinct genotypes, unified by a gene expression profile similar to Ph-positive ALL but lacking the BCR: ABL1 fusion. Previous studies have noted the increased prevalence of Ph-like B-cell ALL in Hispanic patients. Our study evaluates Ph-like B- cell ALL clinical/genomic features and outcomes in a predominantly Hispanic population.
Methods: This is a retrospective chart review of ALL patients that underwent treatment for B-cell ALL at Norris Comprehensive Cancer Center (NCCC) between 2011 and 2023. Identification of fusions associated with Ph-like B-cell ALL was performed using cumulative results from RNA-seq, conventional cytogenetics, and fluorescence in situ hybridization (FISH) with reflex gene fusion transcript analysis. Additionally, we used the Anchored Multiplex PCR™-based multi-gene NGS assay designed to detect known and novel fusions and elevated gene expression levels using a proprietary algorithm in ALL.
Cumulative incidence of relapse (CIR) was evaluated using competing risk regression (Fine-Gray method), with death as a competing outcome. Overall survival (OS) and event-free survival (EFS) were analyzed using Cox proportional hazards model. Events of interest for EFS were relapse, treatment failure, and death. Ph-negative B-cell ALL patients were set as the reference for survival analysis.
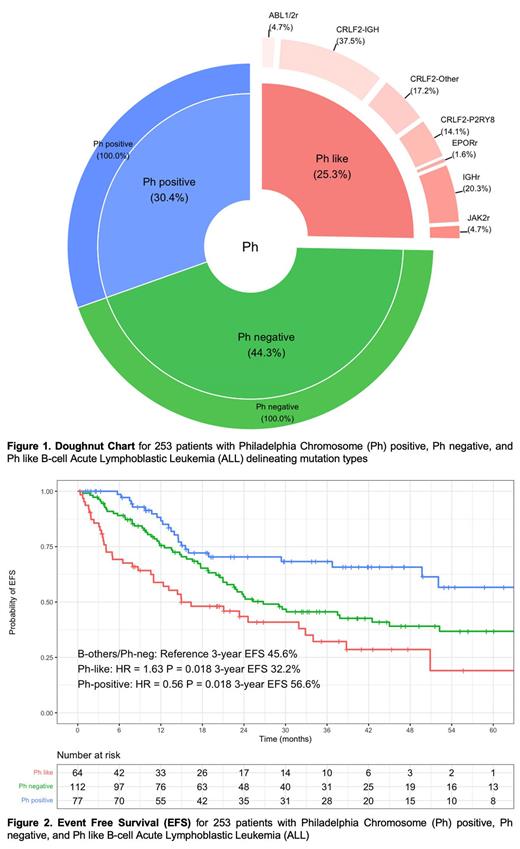
Results: 253 patients were included with a median age at diagnosis of 42 years (range: 18-80). ALL subtypes included 64(25.3%) Ph-like, 77(30.4%) Ph-positive, and 112(44.3%) Ph-negative. Most were Hispanic (N = 186, 73.5%), and the median follow-up time was 27 months. The 3-year OS, EFS, and CIR were 81.3% (95% CI 75.7-87.4%), 49.1% (95% CI 42.7-56.5%), and 39.9% (95% CI 33.0-46.7%).
CRLF2 related mutations constituted 44(68.8%) of Ph-like patients, with 9(14.0%) CRLF2-P2RY8, 24(37.5%) CRLF2-IGH, and 11(17.2%) CRLF2-other gene rearrangements. 19 Ph-like patients had non-CRLF2 mutations consisting of 13(20.3%) IGH, 3(4.7%) ABL1/2, 3(4.7%) JAK2, and 1(1.6%) EPOR rearrangements.
Compared to Ph-negative, Ph-like patients were more likely to have a refractory disease (20.6% vs. 6.2% P=0.006) and require Blinatumomab (67.2% vs. 39.3% P<0.001), with a non-significant trend towards lower rates of CR (84.1% vs 90.9% P=0.21). Ph-like patients had significantly worse EFS (HR = 1.63; 95% CI 1.09-2.45; P=0.018), but similar OS (HR = 0.88; 95% CI 0.39-1.99; P=0.75) and CIR (HR = 1.06; 95% CI 0.65-1.70; P = 0.83). Ph-positive patients displayed improved EFS relative to Ph-negative (HR = 0.56; 95% CI 0.35-0.91; P = 0.018), similar OS (HR = 0.73; 95% CI 0.35-1.50; P = 0.39), and a trend towards improved CIR (HR = 0.67; 95% CI 0.40-1.10; P=0.11). When controlling for age, sex, and treatment type, EFS was worse in Ph-like (HR = 1.57; 95% CI 1.03-2.41; P = 0.037) and improved in Ph-positive (HR = 0.56; 95% CI 0.33-0.93; P = 0.026).
Our incidences of CRLF2 mutations in Ph-like patients aged>40 compared to age ≤40 was (73.3% vs 64.7%, P=0.591). On subgroup analysis of Ph-like patients, univariate regression revealed CRLF2-related Ph-like patients had a worse CIR (HR = 5.68; 95% CI 1.91-16.9; P = 0.002) but similar OS(P=0.99) and EFS(P=0.18). PAX5 expression was also a predictor of poor OS (HR = 8.89; 95% CI 1.06-74.7; P = 0.044) and EFS (HR = 2.51; 95% CI 1.09-5.77; P = 0.031), with a trend towards increased CIR (HR = 2.30; 95% CI 0.92 -5.78; P = 0.075). Compared to non-CRLF2 mutations, CRLF2-Ph-like had worse CIR (HR = 5.68; 95% CI 1.91 -16.9; P = 0.002). Relative to Ph-like patients who achieved MRD negativity during induction, patients who remained MRD positive had worse CIR(HR = 2.92; 95% CI 1.23 -6.94; P = 0.015) and EFS (HR = 4.32; 95% CI 1.890-9.84; P < 0.001). However, after controlling for Blinatumomab administration, the effect diminished (CIR: P=0.73, EFS P=0.28). There were no differences in EFS(P=0.34), CIR(P=0.69), and OS(P=0.36) between Ph-like patients who were transplanted vs not.
Conclusions:
Ph-like B- Cell ALL represents a high-risk disease subtype of adult B-ALL, with poor EFS and frequent treatment failure. CRLF2 translocation confers worse CIR and EFS within Ph-like patients and requires novel treatment approaches.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal